Physiological mechanisms
- Evidence suggests that obesity accounts for up to 90% of the risk of developing type 2 diabetes.
- Not everyone with type 2 diabetes is overweight or obese as defined by Body Mass Index (BMI).
- E.g., indigenous people, South Asians, etc…
- Central adiposity (i.e., intra-abdominal fat) is the underlying issue.



- Adipose (fat) tissue stores much of the excess energy
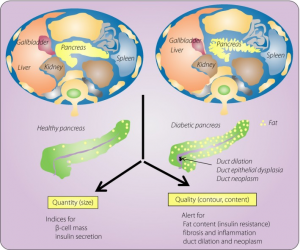
- Excess fat accumulates in other organs → liver, pancreas, and muscle.
- In these non–adipose tissues, excess energy leads to lipotoxicity, meaning the excess fat stored in these cells inhibits their proper functioning.
- This disrupts normal glucose and insulin metabolism.
- Muscle lipotoxicity inhibits glucose uptake.
- This produces peripheral insulin resistance, requiring greater amounts of insulin to “push” glucose into the muscles.
- This resistance is reduced with physical activity as muscle tissues consume energy (e.g., glucose) and become more responsive to insulin.


- Pancreatic lipotoxicity inhibits β-cell insulin production, reducing the amount of insulin available to overcome the insulin resistance in muscles and other organs.
- Significant energy restriction removes triglycerides (fat) from the pancreas in a matter of days, restoring β-cell insulin production.
- This occurs before significant weight loss occurs in other organs and tissues, indicating it is not just excess body fat, but excess energy, driving insulin resistance and type 2 diabetes.
- MRI scans of the pancreas in nearly 33,000 people in the UK.
- Higher pancreatic fat content is associated with a 42% increase in risk of developing type 2 diabetes.
Assessing adiposity
- BMI is not the best measure of excess body fat (adiposity):
– Waist circumference;
– Waist : height ratio;
– Bioimpedance analysis;
– Fat Mass Index =
Fat Mass (kg) ÷ height² (m²).
are much better indicators

