Name of Medicine
Sitagliptin phosphate monohydrate/metformin hydrochloride
Presentation
JANUMET is available for oral administration as film-coated tablets in 3 different strengths containing sitagliptin phosphate monohydrate and metformin equivalent to:
– JANUMET 50 mg/500 mg containing 50 mg sitagliptin and 500 mg metformin JANUMET 50 mg/850 mg containing 50mg sitagliptin and 850 mg metformin – JANUMET 50 mg/1000 mg containing 50mg sitagliptin and 1000 mg metforminKey Practice Points
Therapeutic Indications:
- JANUMET is indicated as an adjunct to healthy eating and physical activity to
improve glycaemic management in adults with type 2 diabetes mellitus when
treatment with both sitagliptin and metformin is appropriate.
For the latest PBS indications for JANUMET please see
https://www.pbs.gov.au/medicine/item/10089B-10090C-9449H-9450J-9451K
Dose:
Life threatening lactic acidosis can occur due to accumulation of metformin. The main risk factor is renal impairment, other risk factors include old age associated with reduced renal function and high doses of metformin above 2g per day.
- The dosage of diabetes therapy with JANUMET should be individualised based on a person’s current regimen, effectiveness and tolerability while not exceeding the maximum recommended daily dose of 100 mg sitagliptin and 2000 mg metformin. (Person centred care)
- JANUMET should generally be given twice daily with meals, with gradual dose escalation, to reduce the gastrointestinal (GI) side effects due to metformin.
- As initial therapy:
– For individuals with type 2 diabetes mellitus, whose hyperglycaemia is inadequately managed with healthy eating and physical activity, when dual therapy is appropriate, the recommended total daily starting dose of JANUMET is 100 mg sitagliptin and 1000 mg metformin hydrochloride. Individuals with inadequate glycaemic management on this dose should have their metformin dose increased up to a maximum of 100 mg sitagliptin/2000 mg metformin hydrochloride daily.
– For individuals inadequately managed on sitagliptin monotherapy: For those whose diabetes is inadequately on sitagliptin alone, the recommended starting dose of JANUMET is 100 mg sitagliptin and 1000 mg metformin hydrochloride daily. Individuals may be titrated up to 100 mg sitagliptin/2000 mg metformin hydrochloride daily to achieve healthy glycaemia. Individuals taking sitagliptin monotherapy dose-adjusted for renal impairment should not be switched to JANUMET.
– For individuals, whose diabetes is inadequately managed on metformin monotherapy: For those whose diabetes is not adequately managed on metformin alone, the usual starting dose of JANUMET should provide sitagliptin 100 mg total daily dose plus the dose of metformin already being taken.
– For individuals switching from sitagliptin co-administered with metformin: For individuals switching from sitagliptin co-administered with metformin, JANUMET may be initiated at the dose of sitagliptin, and metformin already being taken.
– For individuals who diabetes is inadequately managed on dual combination therapy with metformin and a sulfonylurea: The usual starting dose of JANUMET should provide sitagliptin 100 mg total daily dose and the dose of metformin already being taken. Individuals may require lower sulfonylurea doses to reduce the risk of sulfonylurea-induced hypoglycaemia.
Note: Diabetes MedsCheck with counselling on managing hypoglycaemia and referral for blood glucose monitoring.
– For individuals, whose diabetes is inadequately managed on dual combination therapy with metformin and insulin: The usual starting dose of JANUMET should provide 100 mg total daily dose of sitagliptin. In determining the starting dose of the metformin component, an individual’s level of glycaemia and current dose of metformin should be considered. Individuals currently on or initiating insulin therapy may require lower doses of insulin to reduce the risk of hypoglycaemia.
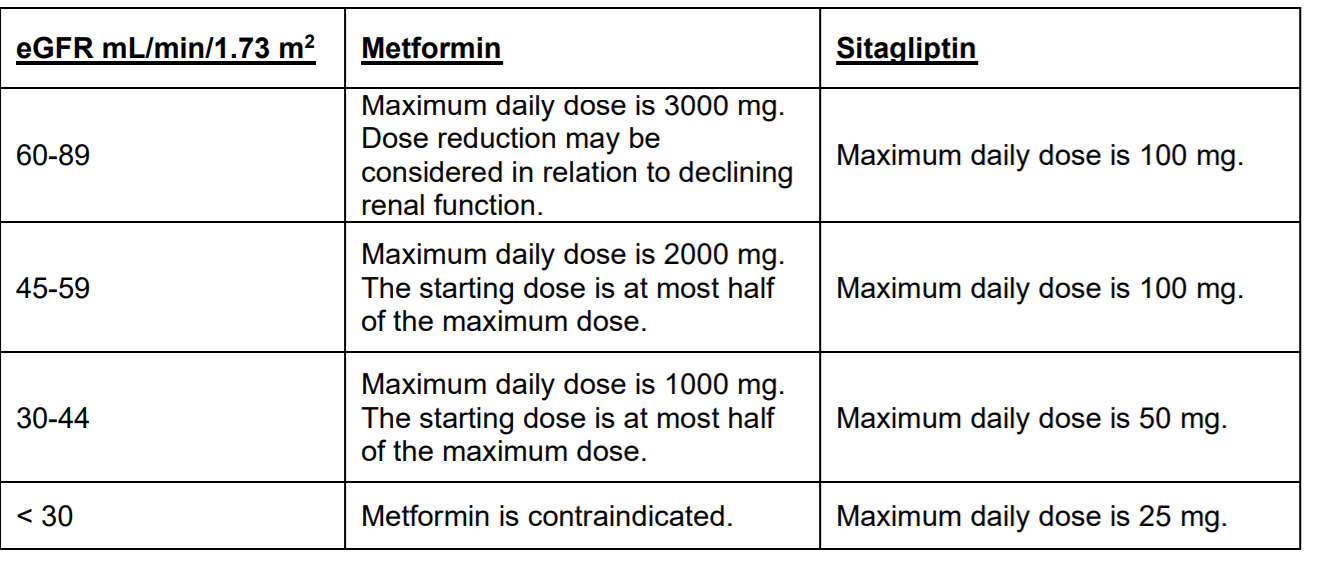
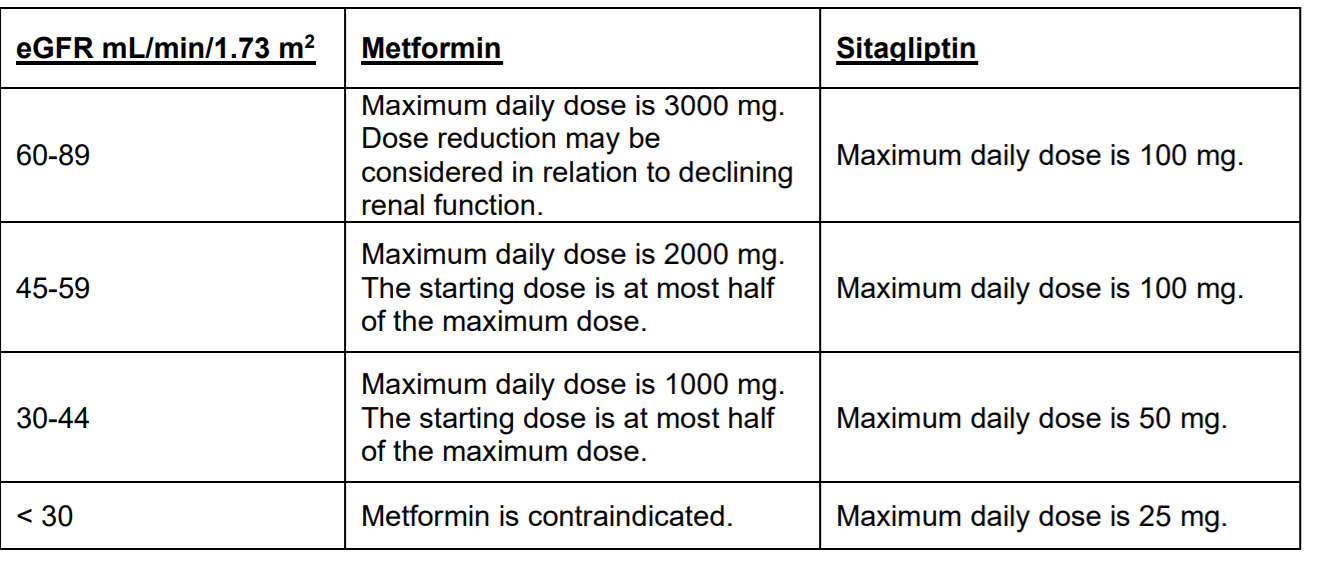
Note: Diabetes MedsCheck with counselling on managing hypoglycaemia and referral for blood glucose monitoring - Renal impairment: No dose adjustment is needed in mild renal impairment (estimated glomerular filtration rate [eGFR] ≥ 60 mL/min/1.73 m2). An eGFR should be assessed before initiation of treatment with JANUMET and at least annually thereafter. In those at increased risk of further progression of renal impairment and in the elderly, renal function should be assessed more frequently, e.g. every 3-6 months.
- The maximum daily dose of metformin should preferably be divided into 2-3 daily doses.
- Factors that may increase risk of lactic acidosis should be reviewed before considering initiation of metformin in those with eGFR < 60 mL/min/1.73 m2
- JANUMET is contraindicated with eGFR < 30 mL/min/1.73 m2
- JANUMET is not recommended in those with an eGFR ≥ 30 mL/min/1.73 m2 and <45 mL/min/1.73 m2 because these individuals require a lower dosage of sitagliptin than what is available in the fixed combination JANUMET product.
- Hepatic impairment
– Sitagliptin phosphate monohydrate: In individuals with moderate hepatic impairment (Child-Pugh score 7 to 9), mean AUC and Cmax of sitagliptin increased approximately 21% and 13%, respectively, compared to healthy matched controls following administration of a single 100 mg dose of sitagliptin. These differences are not considered to be clinically meaningful. There is no clinical experience in individual with severe hepatic impairment (Child-Pugh score > 9). However, because sitagliptin is primarily renally eliminated, severe hepatic impairment is not expected to affect the pharmacokinetics of sitagliptin. – Metformin hydrochloride: No pharmacokinetic studies of metformin have been conducted in those with hepatic impairment. Impaired hepatic function has been associated with some cases of lactic acidosis in those taking metformin, however.
Elderly:
As metformin and sitagliptin are excreted by the kidney, JANUMET should be used with caution as age increases. Monitoring of renal function is necessary to aid in prevention of metformin-associated lactic acidosis, particularly in the elderly.
Children:
JANUMET are not currently indicated for use in children below 18 years.
Contraindications:
- Severe renal impairment (eGFR < 30 mL/min/1.73 m2)
- Known hypersensitivity to sitagliptin phosphate monohydrate, metformin hydrochloride or any other component of JANUMET
- Acute or chronic metabolic acidosis, including ketoacidosis, with or without coma.
- JANUMET should be temporarily discontinued when undergoing radiological studies involving intravascular administration of iodinated contrast materials, because the use of such products may result in acute alteration of renal function.
- Sitagliptin – During post marketing experience the following adverse reactions have been reported with use of serious hypersensitivity reactions, including anaphylaxis and angioedema. Because these reactions are reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency. If a serious hypersensitivity reaction to sitagliptin is suspected, discontinue JANUMET, assess for other potential causes for the event, and institute alternative treatment for diabetes. Note: Diabetes MedsCheck with counselling on side effect profile and referral to healthcare team as required. -Pancreatitis: During post-marketing experience, there have been spontaneously reported adverse reactions of acute pancreatitis. Individuals should be informed of the characteristic symptoms of acute pancreatitis: including persistent, severe abdominal pain. If pancreatitis is suspected, JANUMET should be discontinued. Note: Diabetes MedsCheck with counselling on side effect profile and referral to healthcare team as required. – Bullous pemphigoid: post-marketing cases of bullous pemphigoid requiring hospitalisation have been reported with DPP4 inhibitor use. In reported cases, individuals typically recovered with topical or systemic immunosuppressive treatment and discontinuation of the DPP-4 inhibitor. Counsel individuals to report development of blisters or erosions while receiving JANUMET. If bullous pemphigoid is suspected, JANUMET should be discontinued and referral to a dermatologist should be considered for diagnosis and appropriate treatment. Note: Diabetes MedsCheck with counselling on side effect profile and referral to healthcare team as required. -Arthralgia: There have been post marketing reports of joint pain, which may be severe, in those taking DPP4 inhibitors. Onset of symptoms following initiation of treatment may be rapid or may occur after longer periods. Discontinuation of therapy should be considered in individuals who present with or experience an exacerbation of joint symptoms during treatment with Sitagliptin. Note: Diabetes MedsCheck with counselling on side effect profile and referral to healthcare team as required.
Precautions:
- JANUMET should not be used in individuals with type 1 diabetes mellitus.
- Metformin
- Monitoring of renal function: Renal function should be confirmed before initiation of JANUMET therapy, and then at least once a year in those with normal renal function and at least two to four times a year if serum creatinine levels are at or above the upper limit of normal and in elderly individuals. Decreased renal function in the elderly is frequent and asymptomatic. Special caution should be exercised in situations where renal function may become impaired, for example when initiating antihypertensive or diuretic therapy or when starting treatment with a nonsteroidal anti-inflammatory drug (NSAID). Note: Diabetes MedsCheck with referral for annual cycle of care.
- Alcohol Intake: Alcohol is known to potentiate the effect of metformin on lactate metabolism. Individuals, therefore, should be warned against excessive alcohol intake while receiving JANUMET.
Adverse Effects:
- Metformin -Gastrointestinal disorders: Gastrointestinal symptoms such as nausea, vomiting, diarrhoea, abdominal pain, and loss of appetite are very common (>10%): these occur most frequently during initiation of therapy and resolve spontaneously in most cases. To prevent these gastrointestinal symptoms, it is recommended that this medicinal product be taken in 2 or 3 daily doses. A slow increase of the dose may also improve gastrointestinal tolerability.-Metabolism and nutrition disorders: Lactic acidosis is a very rare (<0.01%) but serious metabolic complication that can occur due to metformin accumulation during treatment with metformin. The onset of lactic acidosis is often subtle and accompanied only by non-specific symptoms such as malaise, myalgia, respiratory distress, increasing somnolence and non-specific abdominal distress. There may be associated hypothermia, hypotension and resistant bradyarrhythmias with more marked acidosis. Note: Diabetes MedsCheck with referral to healthcare team for education on lactic acidosis. -Hepatobiliary disorders: Very rare: liver function test abnormalities or hepatitis requiring treatment discontinuation. -Skin and subcutaneous tissue disorders: Skin reactions such as erythema, pruritus and urticaria have been reported but the incidence is very rare (<0.01%). -Nervous system disorders -Taste disturbance (3 %) is common. -Vitamin B12 Levels: In controlled, 29-week clinical trials of immediate release metformin, a decrease to subnormal levels of previously normal serum Vitamin B12 levels, without clinical manifestations, was observed in approximately 7% of individuals. Such decrease, possibly due to interference with B12 absorption from the B12-intrinsic factor complex is, however, very rarely associated with anaemia and appears to be rapidly reversible with discontinuation of metformin or Vitamin B12 supplementation. Measurement of haematologic parameters on an annual basis is advised in those on JANUMET and any apparent abnormalities should be appropriately investigated and managed. Certain individuals (those with inadequate Vitamin B12 or calcium intake or absorption) appear to be predisposed to developing subnormal Vitamin B12 levels). See interventions for further information.
- Sitagliptin – During post marketing experience the following adverse reactions have been reported with use of serious hypersensitivity reactions, including anaphylaxis and angioedema. Because these reactions are reported voluntarily from a population of uncertain size, it is not possible to reliably estimate their frequency. If a serious hypersensitivity reaction to sitagliptin is suspected, discontinue JANUMET, assess for other potential causes for the event, and institute alternative treatment for diabetes. Note: Diabetes MedsCheck with counselling on side effect profile and referral to healthcare team as required. -Pancreatitis: During post marketing experience, there have been spontaneously reported adverse reactions of acute pancreatitis. Individuals should be informed of the characteristic symptom of acute pancreatitis: persistent, severe abdominal pain. If pancreatitis is suspected, JANUMET should be discontinued. Note: Diabetes MedsCheck with counselling on side effect profile and referral to healthcare team as required. – Bullous pemphigoid: post-marketing cases of bullous pemphigoid requiring hospitalisation have been reported with DPP4 inhibitor use. In reported cases, individuals typically recovered with topical or systemic immunosuppressive treatment and discontinuation of the DPP-4 inhibitor. Counsel individuals to report development of blisters or erosions while receiving JANUMET. If bullous pemphigoid is suspected, JANUMET should be discontinued and referral to a dermatologist should be considered for diagnosis and appropriate treatment. Note: Diabetes MedsCheck with counselling on side effect profile and referral to healthcare team as required. -Arthralgia: There have been post marketing reports of joint pain, which may be severe, in those taking DPP4 inhibitors. Onset of symptoms following initiation of treatment may be rapid or may occur after longer periods. Discontinuation of therapy should be considered in individuals who present with or experience an exacerbation of joint symptoms during treatment with Sitagliptin. Note: Diabetes MedsCheck with counselling on side effect profile and referral to healthcare team as required.
Pharmacokinetic Properties Summary
- The results of a definitive bioequivalence study in people without diabetes demonstrated that the JANUMET (sitagliptin phosphate monohydrate/metformin hydrochloride) 50 mg/500 mg and 50 mg/1000 mg combination tablets are bioequivalent to coadministration of corresponding doses of sitagliptin phosphate monohydrate (JANUVIA®) and metformin hydrochloride as individual tablets. Because bioequivalence is demonstrated at the lowest and highest combination tablet dose strengths available, bioequivalence is conferred to the (sitagliptin/metformin) 50 mg/850 mg fixed dose combination (FDC) tablet.
Absorption:
- After administration of JANUMET tablets with a high-fat breakfast, the AUC for sitagliptin was not altered. The mean Cmax was decreased by 17%, although the median Tmax was unchanged relative to the fasted state. After administration of JANUMET with a high-fat breakfast, the AUC for metformin increased 62%, the Cmax for metformin decreased by 9%, and the median Tmax for metformin occurred 2 hours later relative to the fasted state.
Distribution:
- Sitagliptin phosphate monohydrate: The mean volume of distribution at steady state following a single 100 mg intravenous dose of sitagliptin to people without diabetes is approximately 198 litres. The fraction of sitagliptin reversibly bound to plasma proteins is low (38%).
- Metformin hydrochloride: Metformin is negligibly bound to plasma proteins. At usual clinical doses and dosing schedules of metformin hydrochloride tablets, steady state plasma concentrations of metformin are reached within 24-48 hours.
Metabolism:
- Sitagliptin phosphate monohydrate: Sitagliptin is primarily eliminated unchanged in urine, and metabolism is a minor pathway. Approximately 79% of sitagliptin is excreted unchanged in the urine.
- Metformin hydrochloride: Intravenous single-dose studies in people without diabetes demonstrate that metformin is excreted unchanged in the urine and does not undergo hepatic metabolism (no metabolites have been identified in humans) or biliary excretion.
Excretion:
- Sitagliptin phosphate monohydrate: Following administration of an oral [14C] sitagliptin dose to people without diabetes , approximately 100% of the administered radioactivity was eliminated in faeces (13%) or urine (87%) within one week of dosing. The apparent terminal t1/2 following a 100 mg oral dose of sitagliptin was approximately 12.4 hours and renal clearance was approximately 350 mL/min. Elimination of sitagliptin occurs primarily via renal excretion and involves active tubular secretion.
- Metformin hydrochloride: Renal clearance is approximately 3.5 times greater than creatinine clearance, which indicates that tubular secretion is the major route of metformin elimination. Following oral administration, approximately 90% of the absorbed drug is eliminated via the renal route within the first 24 hours, with a plasma elimination half-life of approximately 6.2 hours. In blood, the elimination half-life is approximately 17.6 hours, suggesting that the erythrocyte mass may be a compartment of distribution.
More Information
For further information on JANUMET please see
https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2010-PI-03939-3&d=202106081016933
